Updated advice says GPs can deregister patients for ‘unrealistic service demands’
GP practices can now consider deregistering patients who have ‘unnecessarily persistent or unrealistic service demands that cause disruption’.
Stating that protecting GP teams’ mental health is ‘as important’ as protecting their physical health’, NHS England has updated guidance on managing unacceptable patient behaviours to also include non-violent abuse.
These include patients:
- Using bad language or swearing at practice staff or other service users;
- Unnecessarily persistent or unrealistic service demands that cause disruption;
- Verbal, non-verbal and environmental slights, snubs and insults which communicate hostile, derogatory or negative messages;
- Behaviours that target a person based on their protected characteristic or belonging to a marginalised group. These can be intentional and unintentional and are based on biases (either conscious and unconscious).
The guidance goes on to say that ‘where a patient has acted inappropriately or unacceptably, the provider will need to carefully consider’ if the incident ‘meets the relevant criteria for removal from the practice patient list’.
In doing so, the practices should take into account ‘the nature and severity of the incident/behaviour, the impact on practice services, staff or other service users and the patient’s own circumstances’, and:
- If the incident does meet the relevant criteria for removal from the practice patient list a practice will need to decide whether it is ‘nevertheless willing to continue to manage its relationship with the patient or proceed with the removal’.
- If the incident does not meet the relevant criteria for removal from the practice patient list, the practice will need to decide ‘how it will manage its continuing relationship with the patient’.
NHS England’s guidance added that removing a patient from the practice list is ‘expected to be an exceptional event’.
Urging GP practices to update their policies on unacceptable behaviours, NHS England said it ‘supports and requests that providers practice policies addressing inappropriate and unacceptable patient behaviours also explicitly include positions on not tolerating any form of discrimination, harassment or victimisation’.
GPs can also approach their indemnity provider for ‘advice on whether to issue a patient with a warning, instigate an acceptable behaviour agreement or remove a patient from the practice list.
How to deregister abusive patients
If a practice wishes to remove a patient it ‘must normally provide the reason for removal in writing to the patient’. It should also have ‘warned the patient in writing that they are at risk of removal’ within the past 12 months.
However, if an incident was bad enough for practice staff or patients to have ‘feared for their safety’, the patient can be immediately deregistered. These incidents must also be reported to the police.
All patient removals ‘must be recorded by the practice, including the reasons and circumstances of the removal’.
Patients ‘may experience difficulties in registering where they have been removed from a practice list’, however, ‘this should not ordinarily be a factor considered by practices when approached by new patients’ – except on the grounds of ‘violence or threatening behaviour’.

Special Allocation Scheme (SAS): Removal of violent patients
The SAS, which aims to protect general practice against violent or aggressive behaviour, is administered through Primary Care Support England (PCSE). The practice must have grounds to show that the individual to be removed from the practice list with immediate effect committed an act of violence, or behaved in such a way that they feared for their safety. This could be against a doctor, partner, member of staff, visitor or patient on the premises. Of note is the fact that in order for a patient to be allocated to the SAS, incidents need to be reported to the police. However, there is no requirement to provide a police incident number or a crime number. In addition, practices are obliged to report the removal of patients to the Care Quality Commission (CQC). The British Medical Association (BMA) guidance Removing violent patients and the special allocation scheme gives more detail and links to relevant documentation and organisations involved in the process. Please note this is separate from the regulations relating to removal of a patient due to an irretrievable breakdown of the relationship.
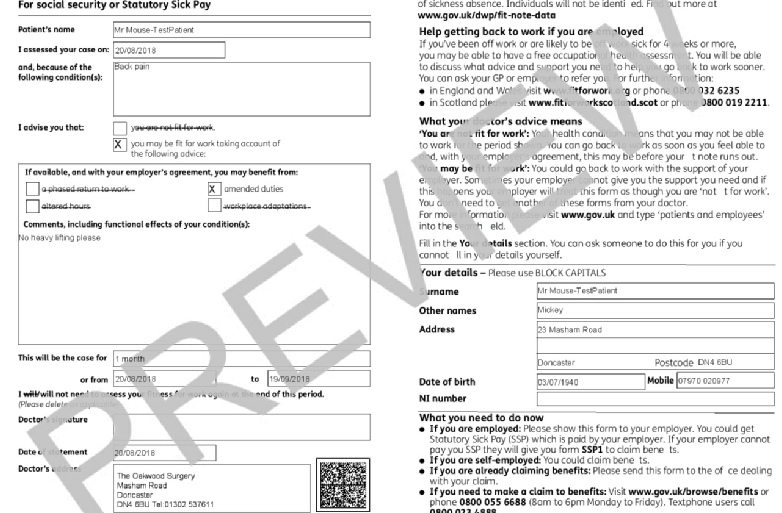
Extending fit note certification
From 1 July, legislation is changing which will allow more healthcare professionals to certify fit notes to patients.
• Currently only doctors can legally certify fit notes. DWP are now changing the legislation which will allow a further four professions to do this. These professions are nurses, occupational therapists, physiotherapists, and pharmacists.
• Not everybody working within these professions should issue fit notes. Professionals should be working in a suitable environment and have the necessary skills and training to have work and health conversations with patients. This task needs to be within their professional ‘scope of practice’, therefore new guidance and training has been developed which will help professionals to identify if this task is suitable for them.
• This legislation change applies across England, Scotland, and Wales.
• This change follows legislation changes in April which removed the need for fit notes to be signed in ink. This change made it possible for doctors to certify fit notes digitally and also for patients to receive their fit note via digital channels (where GP IT systems support this).
General Practice Factual Report (GPFR) pilot
A pilot started last month (May) to trial a replacement to the existing GPFR – also known as DS1500 or the Personal Independence Payment (PIP) form – which GPs are asked to complete to support patients’ claims. The new form is designed to be quicker and easier for GPs to complete, whilst still capturing the information needed. The trial will run for 6 months, and the Department for Work and Pensions (DWP) hopes that GPs will engage with it and provide any helpful feedback and comments they may have on the new form. During the pilot GPs may sometimes receive the existing GPFR and may sometimes receive the version being trialled.
Mentorship Scheme
Doncaster LMC has been running a mentorship scheme to support local GPs for some time now. We have a panel of experienced GPs and their profile and photos are available on the Doncaster LMC website to help you choose the most relevant mentor for your needs Mentors – Doncaster LMC . If you would like free, confidential support please follow this link Apply to be a mentee – Doncaster LMC

Experience General Practice - We need your help.
There are a large number of young people in our area who want to become doctors but cannot get experience.
To be able to study medicine at university you need to demonstrate an understanding of what it means to be a doctor. This requires evidence of time spent in a clinical environment such as in a hospital or general practice.
Doncaster LMC created “Experience General Practice” to provide the opportunity to spend time with local GP teams to help learn what it means to be a doctor. We hope that by exposing young people to General Practice we can inspire our next generation of GPs.
Although we have been running the scheme successfully for some time, we have many more applicants than places available.
I would be grateful if you would consider offering some placements.
For further information please follow the link below, or contact office@doncasterlmc.co.uk
https://www.doncasterlmc.co.uk/experience-gp where you will find advice for practices, a confidentiality agreement and placement offer template.
Practice Vacancies Reminder
If you would like to advertise your practice vacancies you can now place your own advert on the Doncaster LMC website Jobs – Doncaster LMC this ensures that the advert is seen by the largest possible audience.



